Ryan M. Harrison
Pavan Jagalur
Mukundan Srinivasan
Amida Technology Solutions, Inc.
December 2021
Summary
The CMS Interoperability and Patient Access Final Rule (CMS-9115-F) requires commercial payers, Medicaid Advantage plans and state Medicaid agencies to provide a patient access API, which will allow patients to delegate access to their claims and clinical records to third-party applications. While the access and identity landscape vary widely between enterprises, we have identified three integration patterns that will cover most payer use-cases for CMS Patient Access FHIR-API compliance. In this white paper, we use a state Medicaid agency use-case to demonstrate the application of these three integration patterns.
Problem
On May 1, 2020, the CMS1 and ONC2 interoperability rules were published on the Federal Register. These rules require individual patient access (2021) and payer-to-payer exchange (2022) via API (Application Programming Interface) without special effort. The mandates from CMS cover both Medicaid’s Fee-For-Service (FFS) and Medicaid Managed Care Organization (MCO) programs.
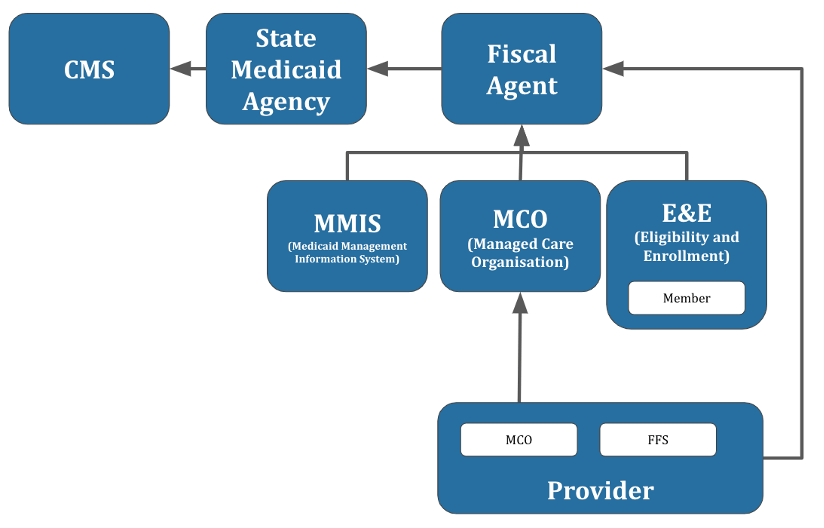
Medicaid programs are administered by 55 distinct state and territorial entities, each of which has its own assortment of IT systems.3 Each state Medicaid program in turn contracts with multiple companies with their own siloed identity system (Figure 1). Hundreds of entities – from state agencies to their contractual partners, including fiscal agents, Medicaid Management Information System (MMIS), Eligibility and Enrollment (E&E), and MCOs – will have to comply with the CMS and ONC interoperability mandates starting in late 2020. For example, Virginia Medicaid has two fiscal agents, four MMIS vendors, two E&E vendors,4 one Enrollment Broker System (EBS) vendor, one FFS Non-Emergency Medical Transportation (NEMT) broker, six state-contracted MCOs, seventeen help desks, and countless FFS providers.
Because of the byzantine identity landscape, a typical Medicaid member could be forced to navigate more than a half-dozen identity systems to enroll and ultimately see a physician. Federated identity systems with SSO offer a solution; a member is provided one login for access to multiple disparate systems. The systems themselves remain siloed, but the member’s identity is shared and administered from one central location.
The Substitutable Medical Apps Reusable Technology (SMART) on Fast Healthcare Interoperability Resource (FHIR) and FHIR Bulk Access standards are the leading mechanisms to facilitate individual access and payer-to-payer exchange. A SMART on FHIR solution for delegated individual access requires, at a minimum, identity management for members and third-party applications. In complying with the CMS and ONC access mandates, state Medicaid agencies have the opportunity to both address the immediate regulatory requirement for member access and to modernize their member identity solutions.
Solution Patterns
Given the heterogeneous identity landscape of state Medicaid agencies, we classify three integration approaches based on the existence of an SSO solution and state-wide Medicaid Member Portal (Table 1).
| Single Sign-On (SSO) | |||
| Yes | No | ||
| State Medicaid Member Portal | Yes | Pattern 1 | Pattern 2 |
| No | Pattern 1 | Pattern 3 |
Pattern 1: Existing SSO
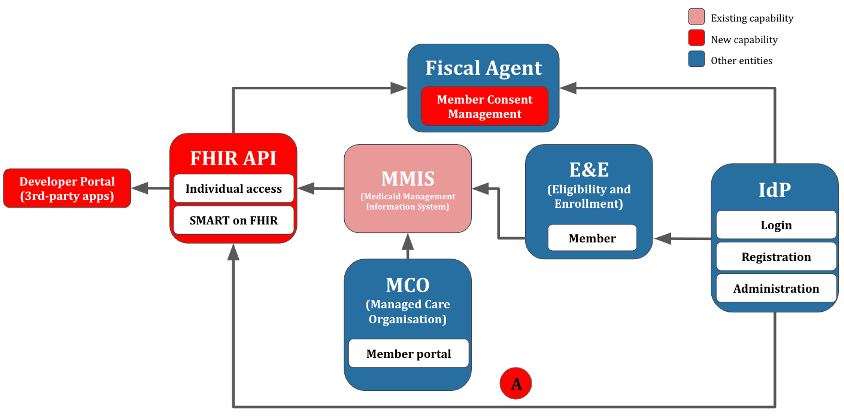
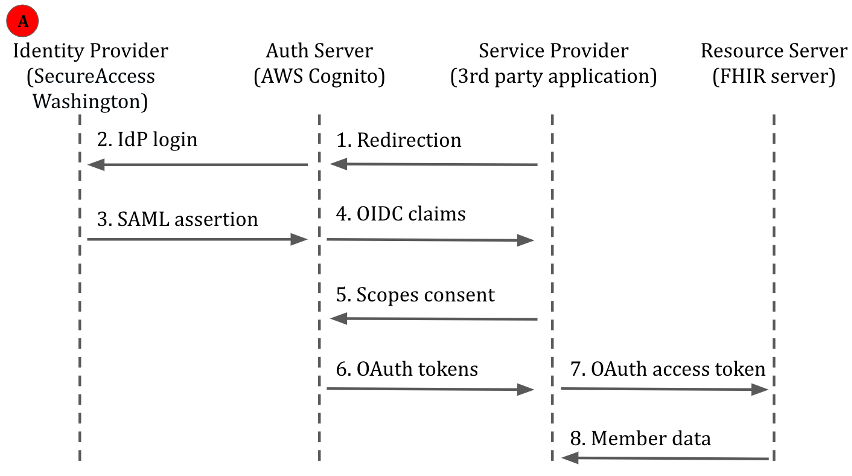
In pattern 1 (Figure 2), the state Medicaid agency integrates with an existing IdP, which may be provided by the state or the state Medicaid agency itself.
SMART on FHIR specifies both authentication and authorization, using OpenID Connect (OIDC) claims (authentication) and OAuth2.0 scopes (authorization). A SMART on FHIR id_token includes OIDC claims; the access_token contains FHIR-specific OAuth2.0 scopes; and the refresh_token is used to request a new access_token without prompting the user for another login.
Rather than add SMART on FHIR scopes to the existing portal, we would federate the identity to a FHIR Auth server. In a federated architecture, the only high-level requirements of the IdP would be to support either OIDC or SAML. To conform with SMART on FHIR, downstream applications would consume identity as OIDC, regardless of whether the upstream IdP used OIDC or SAML.
Solution Building Block: SecureAccess Washington using SAML and AWS Cognito (OIDC)
AWS Cognito, like other identity management solutions, supports both authentication and authorization. Identities are managed via either Cognito User Pools or Identity Pools. Both pool types support federation from OIDC and SAML providers, such as SecureAccess Washington. As Medicaid users would not require direct access to underlying AWS resources, Cognito User Pools are often the more appropriate choice.
A Cognito User Pool may back multiple resource servers, and each can be configured with a distinct set of allowed authorization scopes. The access_token is retrieved with an appropriate OAuth2.0 flow — for example, an “Authorization Code” flow for mobile apps. The service provider – for example, a third-party FHIR application – may then use the access_token for delegated access to a resource server.
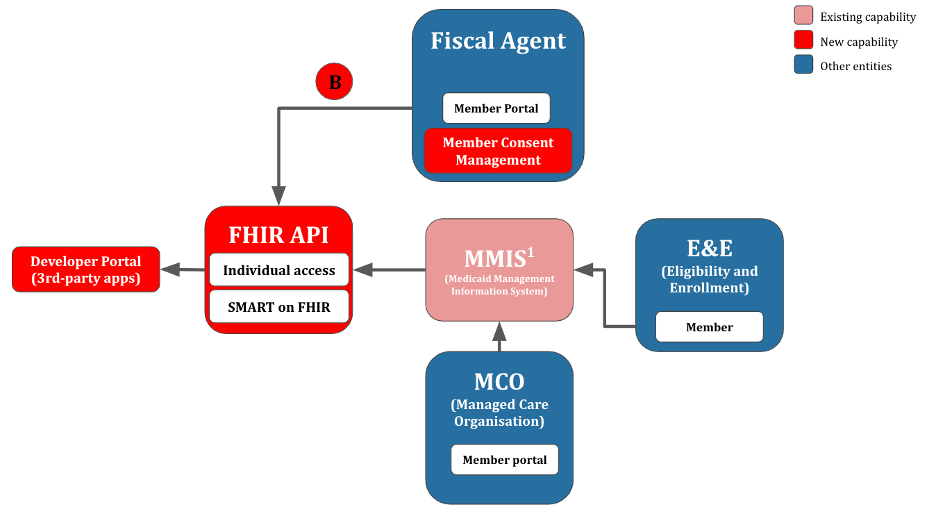
Pattern 2: No SSO, Existing State Medicaid Member Portal
In pattern 2 (Figure 4), no SSO is available, but there is an existing Fiscal Agent member portal. Here, the state Medicaid agency may be able to use the same non-SSO identity as the existing member portal. This represents a stop-gap arrangement that avoids the deployment of a full-fledged SSO solution, at the expense of substantial technical debt. Member consent management can be added to the existing state Medicaid member portal.
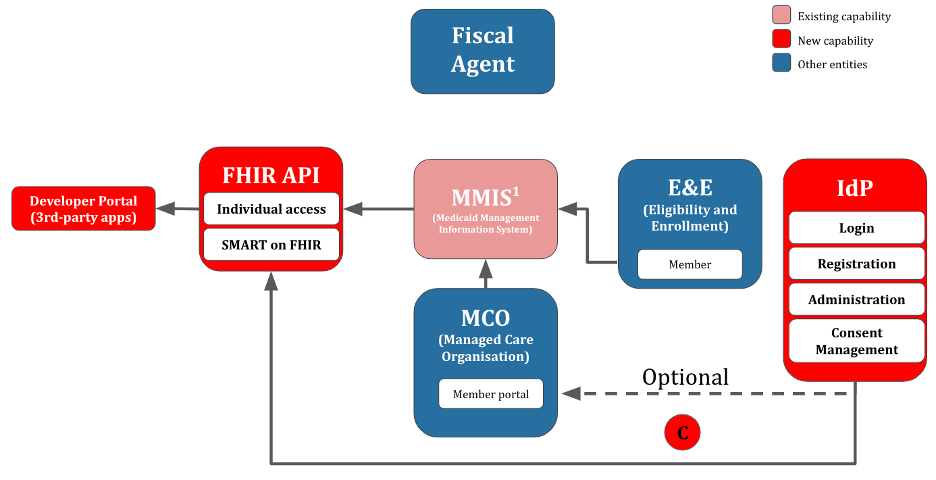
Pattern 3: No SSO, No State Medicaid Member Portal
In pattern 3, neither SSO nor a state Medicaid member portal are available. A less sustainable option would be to build a member directory into the Auth server used by the FHIR server. This would require either: 1) having members create an account before sharing data via FHIR, or 2) provisioning accounts in the Auth server for every member. A more sustainable option (Figure 5) would entail providing an SSO-supporting IdP to the state Medicaid agency, which would be similar to the pre-existing IdP depicted in Pattern 1 (Figure 3).
Although most modern IdPs support the open standards SAML and OIDC, many IdPs remain closed-source. Selecting a FLOSS (Free/Libre and Open-Source Software) IdP avoids vendor-locking both the IdP vendor proper and IdP-related professional services such as integration and long-term support. Further, selecting a FLOSS IdP serves as a form of futureproofing. In a worst-case pattern, where the IdP vendor is either unable or unwilling to support future use-cases, a FLOSS IdP can be unilaterally extended by a state Medicaid agency or integration partner (although this comes at the expense of long-term support for the extension). A common criticism of FLOSS solutions is that they lack enterprise support; however, within the IdP space, enterprise backing is provided by firms such as Apereo (educational institutions), the Open Identity Platform Community, Shibboleth, and Redhat/IBM.
Recommendations
- Use enterprise wide SSO, for your CMS FHIR patient access API solution. Although SAML-based SSO configurations will vary by IdP, integrating with an existing IdP via SAML (Pattern 1) will be much less effort than building an ad hoc solution (Pattern 2) or providing a full-fledged IdP (Pattern 3).
- Integrate consent management with existing member-portal workflows. Members must have a mechanism to revoke consent to third-party applications. Members should also be able to conveniently view their consents and see, at a minimum, the last time each third-party application accessed their data. Consent management can be provided by a stand-alone application linked by SSO; however, administering their account should be seamless to the users. For example, it is more user-friendly to update address, revoke consent, and add a new household member from within one user flow, as opposed to three distinct flows.
- Prioritize FLOSS (Free/Libre and Open-Source Software) and open standards in vendor procurement. Vendor-locking to a closed standard is a death knell to innovation. Indeed, SAML and OpenID Connect (OIDC) were born out of a frustrating landscape of competing proprietary authentication protocols.
- Plan for an increase in HelpDesk activity for third-party access. In pattern 1, members will need to remember their login credentials to consent to third-party access. Expect increased HelpDesk volume for password resets and questions about what information is being shared with third-party providers. First- and second-tier HelpDesk employees will require training on common member inquiries related to FHIR. For third-tier support, an escalation path to your internal development team or contractor will also be needed. User guides, including a FAQ, are recommended for stakeholders such as members, third-party FHIR application developers, and HelpDesk staff.
Appendix: Identity Providers (IdP)
Federal Identity Providers: Login.gov
In the Federal Government, the General Services Administration (GSA)5 has deployed the login.gov SSO portal. Rather than build and support their own identity solutions, federal agencies have the option to use the login.gov SSO.6 Following a one-time integration with login.gov, federal agencies outsource the non-differentiated work of maintaining a secure, National Institute of Standards and Technology(NIST)-compliant identity management solution that automatically stays up-to-date with the latest best practices.
Where token-based authentication is used, establishing a federated Identity Provider (IdP) allows agencies to leverage each other’s personnel security and background investigation processes. This avoids duplicate background screenings, facilitates moves between agencies, and reduces the use of policy exemptions to Multi-Factor Authentication (MFA) requirements when generating temporary accounts. In short, smoother end-user interactions (e.g. obviating the need to juggle multiple logins), better security (e.g. built-in identity-proofing and MFA), lower cost (e.g. amortizing the expense of the identity management system over many agencies), and the facilitation of cross-agency knowledge-sharing (e.g. reusing software components from other agencies). Although login.gov does not support state and local users, it nonetheless serves as a reference model for SSO within government.
State Identity Providers: North Carolina, Washington, Michigan
At the state level, North Carolina has introduced the North Carolina Identity Management Service (NCID) for state and local SSO.7 Importantly, the NCID system supports state and local employees, as well as individual citizens and business users, within the same SSO system. NCID supports SAML 2.0.8
The state of Washington hosts two distinct SSO systems — Enterprise Active Directory9 for state and local employees, and SecureAccess Washington (SAW)10 for the general public. For example, Washington Connection (cash assistance, food assistance), Unemployment and Licensing (including motor vehicles) uses SAW to authenticate the general public. Washington Healthplanfinder (Medicaid, CHIP) does not appear to use SAW on its public site. Cloud-hosted agency applications using SAW must authenticate via SAML 2.0.
Michigan hosts the general-public-facing MILogin11 SSO system, which supports both individual Michigan citizens and businesses/organizations. MIBridges, the state’s consolidated benefits portal (Medicaid, cash assistance, childcare, emergency relief, food assistance), uses MILogin. Michigan Medicaid’s myHealthPortal (web) and myHealthButton (mobile) applications also use MILogin.12
| Product | Vendor | Licensing | Notes |
| Login.gov | US Government | Closed source | Production availability for Federal agencies. Pilot availability for state and local governments.13 |
| MILogin | Michigan | Closed source | Used by MIBridges, which includes Michigan Medicaid. |
| NCID | North Carolina | Closed source | |
| SecureAccess Washington | Washington | Closed source | Used by Washington Connection assistance programs. |
| Auth0 | Auth0 | Closed source | |
| AWS Cognito | AWS | Closed source | Lacks some governance and user-management features commonly found in identity management solutions. Does not support SMART on FHIR.14 |
| Igia on Keycloak | Persistent | Open source | Specific to SMART on FHIR. |
| Keycloak Redhat-SSO | Redhat | Open source | Keycloak is the community-supported upstream, while Redhat-SSO is the enterprise-supported downstream. |
| IBM IAM | IBM | Closed source15 | |
| Okta | Okta | Closed source | Used by CMS Quality Payment Program. Okta has an unofficial and unsupported SMART on FHIR reference implementation.16,17 |
Overview of Identity Protocols
Recall that authentication is about who the user is, and authorization is about what a user is allowed to do. Identity providers and identity protocols address the who; JSON Web Token (JWT) scopes, such as those used in SMART on FHIR, address the what.
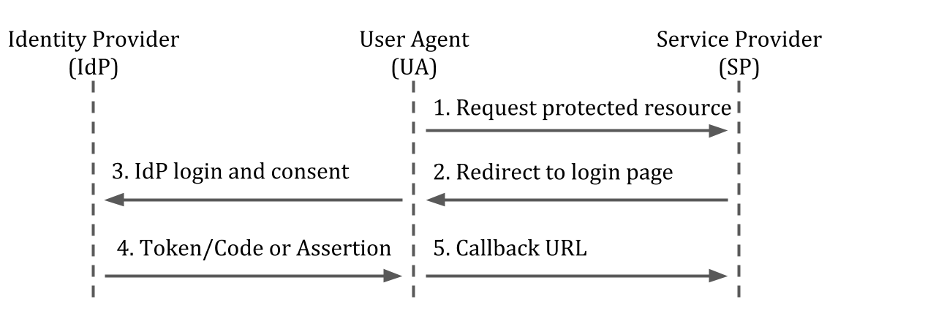
Lightweight Directory Access Protocol (LDAP), OpenID Connect (OIDC), and Security Assertion Markup Language (SAML) are three common authentication protocols. These protocols are used to authenticate transactions between a User Agent (e.g. an internet browser), a Service Provider (e.g. a web application), and an Identity Provider (which includes a directory service)(Figure 6). LDAP is most commonly used for on-premises applications (e.g. signing into a remote desktop), whereas SAML and OIDC are most commonly used for web applications. In practice, most enterprises will use both LDAP (SSO for employees)18 and SAML/OIDC (SSO for customers).