Ryan M. Harrison
Henry Mayen Velasquez
Matthew McCall
Amida Technology Solutions, Inc.
December 2021
Summary
HL7 FHIR (Fast Healthcare Interoperability Resources) is a “platform specification” for health data exchange. An important enabler of data exchange is access control, specifically AuthN (authentication: who are you?) and AuthZ (authorization: what are you allowed to do?).
We provide an overview of SMART on FHIR, the de facto standard for role-based access control (RBAC) with FHIR. Since there is no standard for attribute-based access control (ABAC) with FHIR, we discuss available implementations.
Although we briefly recap the most essential topics in footnotes, this white paper assumes an introductory understanding of RBAC versus ABAC access control and FHIR.
Role-Based Access Control with “SMART on FHIR”
Access control is comprised of two actions, authentication (AuthN) and authorization (AuthZ). Authentication is the process by which a system verifies the identity of an individual or resource requesting access. Authorization is the process to ensure that authenticated requests access the appropriate resources.
Role-based access control (RBAC) defines a set of roles and permissions. Users are assigned roles — e.g., “system administrator,” “team lead,” or “member.”1 Each role is assigned a set of permissions — e.g., read and write access to a resource.
Using RBAC in practice requires a system of record for users, as well as a way to encode permissions and roles, which is what Substitutable Medical Applications, Reusable Technologies (SMART) is designed to provide. In this context, “SMART on FHIR” is a marketing term that refers to Open ID (AuthN) and OAuth 2.0 (AuthZ) with FHIR resources.2
To confuse matters, like with the term “HL7,” the meaning of SMART changes depending on context. HL7 may refer to the Health Level Seven organization, the HL7 v2 messaging specification, or, less commonly, other specific projects such as HL7 v3 messaging, HL7 FHIR, or HL7 CDA. In the same way, SMART may refer to the specification for using OpenID and OAuth 2.0 with FHIR resources (our usage), the specific FHIR implementation guide (SMART Application Launch Framework Implementation Guide3), the non-profit organization “SMART Health IT project,” or the collaboration between the SMART Health IT project and the Argonaut project, which drives adoption of the specification among electronic health record (EHR) vendors and the app community.
OAuth 2.0 defines a protocol for the exchange of tokens. JSON Web Tokens (JWTs4) are a specific encoding for tokens. JWTs are a convenient token format for distributed web applications because they can be verified by client applications — i.e., they require no additional server-side verification or look-up. A JWT has three parts: header, payload, and signature.
The header contains the cryptographic signing algorithm (alg)5 and token type (typ). The payload contains claims, most importantly authorization permissions (scope) and expiry time (exp). The signature allows a client to independently verify that the JWT, and thereby the JWT’s claims, have not been tampered with.6
JWT scope Claim
The JWT specification does not specify how the scope claim is encoded.7 Here, the innovations of SMART on FHIR are 1) separating “patient” and “user” namespaces, 2) tying the scope authorization permissions directly to FHIR resource types, and 3) standardizing the scope format for FHIR applications.
The SMART on FHIR Implementation Guide distinguishes between “patient-specific” and “user-level” interactions.8 A permission prefixed with patient/ concerns one and only one patient, while a permission prefixed with user/ concerns all administrative functions to which that user has access. For example, viewing one’s own personal health record would use a patient/ prefixed permission, while viewing a listing of all patients on a nurses’ ward would use a user/ prefixed permission.
SMART on FHIR restricts access within patient/ and user/ by resource type. For example, patient/Patient.write allows write access to the Patient resource type for a specific patient. This would include the POST, PUT, PATCH, and DELETE REST verbs. Meanwhile, user/Observation.read allows read access to the Observation resource type for all observations the given user has access to. This includes the GET and HEAD REST verbs.
Taken together, the scope standardization of permissions takes the form:
patient/:resourceType.(read|write|*)
user/:resourceType.(read|write|*)
… where :resourceType is a single FHIR resource. Commonly scoped FHIR resources include Claim, ExplanationOfBenefit (EOB), Patient, Practitioner, Observation and Organization.
Example with SMART on FHIR access token
JWTs are generic and can be used for all the common token types: access_token, id_token (identity token), and refresh_token. Here, we demonstrate a worked example of a SMART on FHIR access_token used for authorization.
Base64 serialized access_token, with the format header.payload.signature:
eyJ0eXAiOiJKV1QiLCJhbGciOiJIUzI1NiJ9.eyJpc3MiOiJodHRwczovL2Voci5leGFtcGxlLmNvbS9maGlyIiwiaWF0IjoxNTYzMjI3NzQ5LCJleHAiOjE1OTQ3NjM3NDksImF1ZCI6Im15c21hcnRvbmZoaXJhcHAuZXhhbXBsZS5jb20iLCJzdWIiOiJteXVzZXJAbXlzbWFydG9uZmhpcmFwcC5leGFtcGxlLmNvbSIsInNjb3BlIjoib3BlbmlkIGZoaXJVc2VyIHBhdGllbnQvKi5yZWFkIn0.BXs6kt7nrMxGEkOGUtUeZt34smU6Mdt1VjHzrX2QoUg
With the de-serialized contents:9
Header
{
“typ”: “JWT”,
“alg”: “HS256”
}
Payload
{
“iss”: “https://ehr.example.com/fhir”,
“iat”: 1563227749,
“exp”: 1594763749,
“aud”: “mysmartonfhirapp.example.com”,
“sub”: “myuser@mysmartonfhirapp.example.com”,
“scope”: “openid fhirUser patient/*.read”
}
Signature
{
HMACSHA256(base64UrlEncode(header) + “.”
+base64UrlEncode(payload), secret <SMARTonFHIR>)
}
This allows access to an id_token (scope: openid fhirUser) and all patient data (scope: patient/*.read).
Limitations of SMART on FHIR
It is important to remember that the original Argonaut use cases for SMART on FHIR were connecting patient- and clinician-centric applications to EHRs. That initial scope has been clarified to include launch profiles (launched from within an EHR or standalone), online_access, and offline_access (allows refresh_token requests).10
The needs of payers and the healthcare industry’s transition toward value-based care (VBC) contracting are outside the scope of SMART on FHIR. VBC falls within the remit of the HL7 Da Vinci project,11 whereas other payer-specific use cases may not have a designated project or working group. Payer use cases that overlap the patient- and practitioner-specific workflows envisaged by SMART on FHIR may be supported, but this must be evaluated on a case-by-case basis.
These overlapping use cases require interaction with one record (personal health record) or a relatively small number of records (practitioner). Therefore, bulk transfer — e.g., provider-to-provider or provider-to-payer transactions with millions of records — are outside the scope of SMART on FHIR.
While simple queries are supported via GET requests with query parameters on resources,12 and across resources via the Search resource type,13 there is not yet a standard for complex queries with conditionals within FHIR or SMART on FHIR.14
SMART on FHIR relies upon RBAC at the FHIR resource level of detail. It allows permissioning by resource type — e.g., patient/Patient.read vs. patient/AllergyIntolerance.read. FHIR has a security model that includes designations for business-, individual-, and patient-sensitive data at the resource level. Neither FHIR nor SMART on FHIR specifies how to use these security designations. Further, SMART on FHIR does not allow restrictions based on attribute within a resource type — e.g., Patient.maritalStatus. Nor does it allow conditional restrictions by either resource or attribute — e.g., allow Medication if Medication.identifier is not protected.15
Attribute-Based Access Control
Attribute-based access control (ABAC) grants rights to the user via policies. Policies are almost always at the attribute level and usually allow conditional statements — e.g., allow <X> if <Y>). eXtensible Access Control Markup Language (XACML) is the de facto standard policy language. Because XACML is cumbersome to write directly, policies are in practice authored with a GUI editor16 or transpiled from pseudocode such as Abbreviated Language for Authorization (ALFA).17
To the best of our knowledge, there is no reference implementation for ABAC with FHIR.18 FHIR does provide the Security resource type and SecurityLabel concept, which could be used in an ABAC control flow. Indeed, the FHIR R4 documentation for SecurityLabel explicitly states, “Local agreements and implementation profiles for the use [of] security labels should describe how the security labels connect to the relevant consent and policy statements.”19
Additionally, an AuditEvent resource type20 is available to maintain an access control log, which is a feature of all mainstream ABAC solutions. Both Security and AuditEvent are at trial use in FHIR R4.
FHIR usually relies on an implementation guide to specify CodableConcepts and ValueSets specific to an application or localization. For example, the US Core implementation guide provides resource profiles with localization to US Office of the National Coordinator for Health IT (ONC) guidelines.21 Security differs in that it relies directly upon the Healthcare Privacy and Security Classification System (HCS) for the five supported security labels. We suspect this choice was made because, while the label categories are enumerated by HCS, their highly localized use would make an implementation guide rather narrow in scope.
As of R4, security labels are ascribed in the metadata of resources.
“resource”: {
“id”: “1”,
“meta”: {
“security”: [{system, code, display}, …]
}
}
Indeed, SecurityLabel can only be applied to the entire resource, not to individual attributes. For example, the Medication resource for the antidepressant Lexapro could have a SecurityLabel applied — e.g., Sensitivity Category, MH (mental health information sensitivity). This use of SecurityLabel is appropriate because each of a patient’s medications are separate resources.
However, because most FHIR resource attributes do not allow arbitrary metadata (for example, in the Medication resource type, there is nowhere within Medication.identifier or Medication.code to append meta.security), there is currently no supported way to encode attribute-level security labels.
{
“resourceType”: “Medication”,
“identifier”: [{ Identifier }], // Business identifier
“code”: { CodeableConcept }, // Taxonomy codes
…
}
As of FHIR R4, SecurityLabel has no facility for conditionality — e.g., allow access IF.
Broadly, ABAC on FHIR could be encoded within FHIR objects or outside FHIR objects. Within FHIR objects, the most obvious paths forward are encoding security labels for attributes within resource.meta or using a new FHIR resource type. Security labels within the FHIR resource metadata are advantageous because they would be sent with the resource by default at exchange. For example, a hypothetical Patient.meta.security.attributes.gender could encode a Sensitivity Category (GENDER: gender and sexual orientation information sensitivity) specific to gender identity, rather than covering the entire Patient resource. The downside of this approach is that it requires updating the base FHIR specification, or authoring one or more custom profiles or extensions.
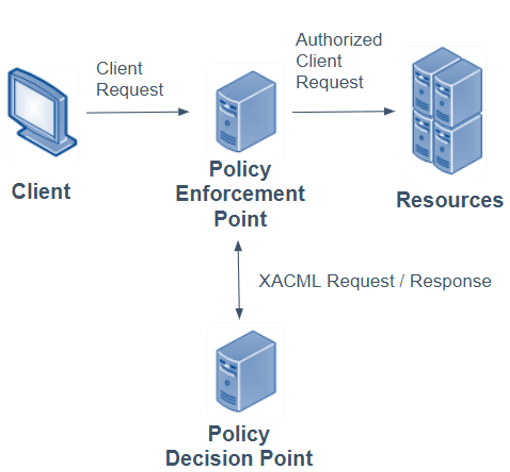
For encoding outside FHIR objects, the most obvious path forward is a FHIR-specific PIP within an ABAC implementation, which allows reuse of the PEP and PAP (Figure 1). Indeed, a literature review reveals this approach in the 2017 paper “Attribute Based Access Control for Healthcare Resources.”22 Briefly, the authors describe their custom integrations with the WSO2 Identity Server, specifically their writing a PIP with XACML encodings of FHIR resource attributes. The advantage and downside of this approach is that it operates outside the FHIR specification — i.e., the policy would not be communicated in a FHIR exchange.
Hybrid RBAC/ABAC approaches are also possible. For example, Janki et al. describe a hybrid approach using a LoopBack proxy server between the client application and the FHIR resource server (HAPI FHIR) that enforces resource-level security labels at the proxy.23